Patient Education
Diverticular Disease
What is Diverticular Disease?
Diverticular Disease is a group of conditions that include diverticulitis, diverticulosis, and diverticular bleeding. Diverticular disease affects men and women at similar rates and the risk of disease increases with age – especially for those over 40. Populations in developed countries are more likely to have diverticular disease.
Key Definitions – Diverticular Disease
A person with diverticular disease may have diverticulosis, diverticulitis, or diverticular bleeding.
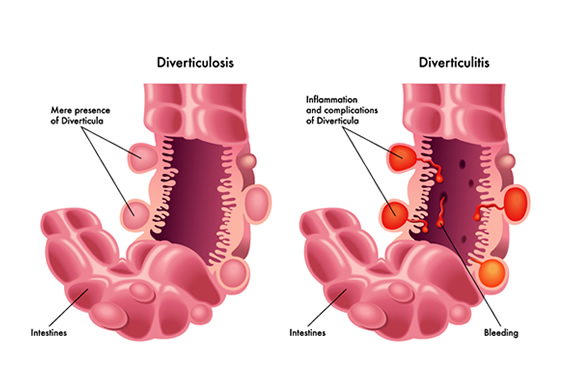
Diverticula / Diverticulum
Small pockets that form in the wall of the bowel. Diverticula is plural (more than one) and Diverticulum is singular (one pocket).
Diverticulosis
The formation of diverticula in the lining of the bowel. Diverticula can be small (pea-sized) or larger. The formation occurs because of increased pressure from fluid, waste, or gas on weak spots of the bowel wall.
Diverticulosis is common but rarely causes symptoms or problems during a patient’s lifetime. It’s found most often during a test for other reasons like a colonoscopy or sigmoidoscopy.
Diverticulitis
When one or more diverticula become infected or inflamed. This occurs most often when waste blocks the small pockets which allow bacteria to multiply and develop into an infection.
Diverticular Bleeding
When a small artery in a diverticulum breaks into the colon. Diverticular bleeding is usually painless and causes bleeding from the rectum. Patients may see maroon or bright red blood during bowel movements.
Diverticulosis Symptoms
Typically, Diverticulosis has no symptoms. It’s possible some may feel tenderness in the area or experience abdominal cramping.
Diverticulitis Symptoms
Symptoms of diverticulitis include:
- Painful cramping which may persist for days. Often pain is felt in the left lower abdomen.
- Tenderness in the lower abdomen
- Nausea / Vomiting
- Fever / Chills
- Constipation
- Diarrhea
You should see a doctor if you have persistent, painful abdominal pain. Schedule an appointment.
Diverticulitis Complications
Complications from diverticulitis are often the result of a tear or perforation in the wall of the intestine. This allows waste from the intestine to leak into the abdominal cavity. This can cause:
- Abscess — a collection of pus in the sack
- Fistula — an abnormal passageway between two areas not normally connected, such as the bowel and bladder
- Obstruction — a blockage in the colon
- Peritonitis — infection as a result of a tear or perforation in the wall of the intestine. This allows waste from the intestine to leak into the abdominal cavity. Peritonitis is a serious condition requiring immediate care.
- Sepsis — a bodywide infection that can lead to failure of multiple organs
Diverticulitis Risk Factors
There are several risk factors that can affect the likelihood of developing diverticulosis:
- Age: People over 40 are more likely to develop diverticulosis.
- Obesity: People who are significantly overweight are at increased risk of developing diverticulosis.
- Smoking: Smoking cigarettes increases your risk of diverticulosis compared to non-smokers.
- Lack of exercise: Exercise has shown to lower risk of diverticulosis.
Diagnosing Diverticulosis
Since most don’t experience symptoms, Diverticulosis is often found during medical procedures done for other reasons. Examples include routine colon cancer screenings such as a colonoscopy or examination for rectal bleeding or abdominal pain.
Diagnosing Diverticulitis
Diverticulitis is normally found during an acute attack. Because there are many causes of abdominal pain, your doctor will rule out other conditions first.
Your doctor may recommend the following tests:
- Blood Tests
- Pregnancy Test
- Liver enzyme test
- Stool test
- CT Scan
Diverticulosis Treatment
Those with diverticulosis who don’t have symptoms don’t need treatment. Doctors typically recommend adopting a high-fiber diet. Eating more fiber could possibly prevent additional diverticula from forming.
It was previously thought that eating seeds, nuts, and corn could lead to diverticulitis. However, there is no scientific evidence of this. Doctors no longer recommend that patients avoid eating seeds, nuts, or corn.
Diverticulitis Treatment
Treatment of diverticulitis will depend on the severity of your symptoms.
Mild Symptoms
For mild diverticulitis symptoms, home treatment may be all that is required. Home treatment may include:
- Antibiotics – Antibiotics may be used to treat the infection. In some mild cases, antibiotics may not be necessary.
- Clear Liquid Diet – To give your bowels a break, your doctor may recommend a clear liquid diet. This will allow your bowel to heal. As symptoms improve you can begin to gradually add solid foods.
- If you develop a fever higher than 100.1ºF, abdominal pain, or are unable to tolerate liquids you should see a doctor. Schedule an appointment.
Severe Symptoms
For severe symptoms of diverticulitis, hospital care may be necessary. This may include:
- Intravenous antibiotics and fluids. Patients do not eat or drink during this treatment, removing as much pressure on the bowels as possible.
- Abscess draining – If an abscess or colon blockage occurs, the doctor may need to drain the site. This is usually done with a small drainage tube placed through the abdomen, rectum, or vagina.
Diverticulitis Surgery
Surgery for Diverticulitis may not be necessary if you improve with medical treatment. If you develop an abdominal infection (Peritonitis) it will usually require surgery.
Types of Diverticulitis Surgery
Resection
In this procedure, the surgeon removes the diseased portion of the intestine and reconnects the healthy areas. In more mild cases, this surgery can be performed using less invasive laparoscopic techniques. This type of resection is often used in non-emergency cases.
Resection & Colostomy
If the intestinal inflammation is too great, it may not be possible to reconnect the healthy portions of your colon to the rectum after removing the diseased portion. In this case, the surgeon will create a colostomy. A colostomy creates an opening (stoma) in your skin that connects to the colon. Waste flows through the opening and collects in a bag.
After a few months, inflammation should be reduced enough to surgically reconnect the colon and allow waste to flow normally through the rectum. The stoma is closed and colostomy bag removed.
Preventing Diverticulosis
Improving the health of your bowel is the best preventative measure for diverticulosis. That includes:
- Consuming 20 to 35 grams of fiber each day
- Avoiding constipation and straining during bowel movements
- Drinking eight 8-ounce glasses of water a day
- Exercising most days
What Causes Diverticular Disease?
Nobody knows the exact cause of diverticular disease, but researchers think certain factors could contribute, like:
- Genetics – Research suggests that diverticular disease may be passed down genetically.
- Lifestyle – Some lifestyle factors may contribute to diverticular disease, including:
- A low fiber diet that is high in red meat
- Not enough physical activity
- Obesity
- Smoking
- Some medications, like NSAIDs
- Bacteria trapped in diverticula
- Changes in the gut microbiome
- Immune system issues
- Connective tissue, muscle, or nerve problems
What’s the Best Diet for Diverticulosis?
If you eat a lot of red meat or have a low fiber diet, your doctor may recommend you cut back on
the red meat and increase your dietary fiber intake. The Dietary Guidelines for Americans, 2020-2025 recommendation is to aim for about 25 grams of fiber for women and 34 grams for men. You can achieve this by adding 1/2 cup of cooked beans, 2-3 pieces of fruit, and a large helping of spinach to your daily meals.
And always drink plenty of fluids to prevent constipation, especially if you increase your fiber intake.
You may find that certain foods seem to cause you symptoms. Tracking your symptoms in a food journal can help you discover what foods trigger diverticulitis symptoms.
What Foods Aggravate Diverticulosis?
In the past, doctors recommended avoiding corn, nuts, seeds, and popcorn, but those guidelines are outdated. Those foods typically don’t get caught in diverticula or cause flare-ups of diverticulitis.
Diverticulosis FAQ
Are Diverticulitis, Diverticulosis, and Diverticular disease the same thing?
No. Diverticulosis is the formation of diverticula, Diverticulitis is when diverticula become infected or inflamed, and Diverticular disease is the blanket term to describe both conditions.
What causes diverticulitis?
Researchers aren’t certain what causes diverticulosis to progress to diverticulitis. It may be due to feces, food, or bacteria becoming lodged in the diverticula.
What is the best treatment for diverticulosis?
Diverticulosis usually doesn’t have any symptoms and doesn’t require treatment. You may need treatment if you develop diverticulitis, however.
Diverticulosis vs. diverticulitis: What’s the difference?
With such similar names, it’s easy to confuse the two. Diverticulosis means that small pockets have formed in the wall of your intestine. You might not even know they are there. But if one or more of those pockets becomes inflamed or infected, you have diverticulitis. It’s possible to have diverticulosis and never develop diverticulitis.
Diverticular Disease Testimonials
“I am a patient of Doctor John Cunningham and l am so very thankful for his expertise and his listening ear!! I am so very grateful that he recommended me to have an Endoscopy and a Colonoscopy together and finally l know why l have been having at times pain in my left side and very ill. I have Diverticular Disorder and Gerd and will see him again in January 2022 to discuss a plan to help me learn better eating habits!!” -Sheila
“I was referred to Dr. MCMyler by my primary care doctor. She treated me for diverticulitis and performed my colonoscopy/endoscopy. At my follow-up visit, Dr. McMyler was warm and caringly answered all my questions. I would recommend her to my friends.” -Paula